Dr Siva has a special interest and many years of expertise in pelvic organ prolapse, including vaginal prolapse and uterine prolapse. He provides wide ranging assessment and treatment and surgery for all kinds of vaginal prolapse and pelvic organ prolapse, including surgery for recurrent vaginal wall prolapse and vaginal vault prolapse surgery.
Dr Siva also performs fertility preserving procedures for women who wish to retain their uterus (including Sacrocolpopexy and Manchester Operation), as well as providing options for conservative, non-surgical management of prolapse.
Types and causes of prolapse
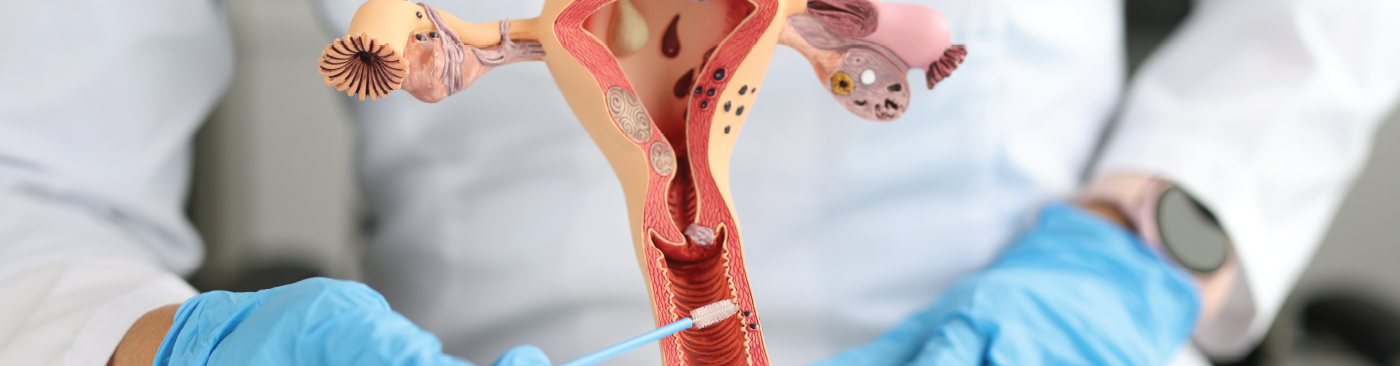
Pelvic organ prolapse (POP) – also known as vaginal prolapse or prolapse – occurs when the connective tissue in your pelvic floor becomes weaker.
As the structure of your vaginal walls lose tone, one or more of the pelvic organs (the bladder, uterus, bowel and/or rectum) may slip down, causing the top of your vagina to weaken, fall into your vaginal canal and sometimes even bulge out.
Cystocele (anterior prolapse) is the most common kind of prolapse and is a prolapse of the bladder into the vagina
Vaginal vault prolapse (vault prolapse) is prolapse of the vaginal wall.
Uterine prolapse (uterovaginal prolapse) occurs when the uterus slips down into or protrudes out of the vagina.
Enterocele (small bowel prolapse) occurs when the small intestine (small bowel) descends into the lower pelvic cavity and pushes at the top part of the vagina, creating a bulge.
Rectocele (rectum prolapse or posterior prolapse) occurs when the end of the large intestine (rectum) pushes against and moves the back wall of the vagina.
Pregnancy, labour, and childbirth (especially multiple vaginal deliveries) are the most common causes of prolapse, however menopause, age, obesity, uterine fibroids, genetic factors and respiratory conditions with a chronic cough can also cause prolapse.
Symptoms and stages of pelvic organ prolapse
Symptoms of prolapse may include a feeling of a vaginal bulge, a vaginal lump, fullness or something coming down or out the vagina, lower back pain, difficulty emptying the bowel or bladder or problems with sexual intercourse.
Some women do not have any symptoms at all and only discover they have a prolapse during a routine gynaecological exam.
These are the four stages of pelvic organ prolapse:
- Stage 1: Your organs are still fairly well supported by your pelvic floor.
- Stage 2: Your pelvic floor organs have begun to fall, but are still inside your vagina.
- Stage 3: Your pelvic floor organs protrude through the opening of your vagina.
- Stage 4: Your pelvic floor organs have fallen right through your vaginal opening.
Pelvic organ prolapse surgery versus non-surgical management of prolapse
Where possible, Dr Siva will provide you with options for conservative management of prolapse, including pelvic floor exercises, seeing a pelvic floor physiotherapist or vaginal pessary insertion.
Surgery for pelvic organ prolapse/vaginal prolapse is usually only recommended if your prolapse is symptomatic.
Dr Siva will assess whether you might require surgery or whether one of the conservative management options will be sufficient to treat your prolapse.
Types of pelvic organ prolapse surgery
The right type of surgery for you will depend on your type of prolapse, the level of prolapse and your overall health and medical history.
Colporrhaphy (vaginal wall repair) – is a reconstructive surgery for patients with stage one or stage two prolapses who have not had other prolapse surgery.
Dr Siva performs this procedure through your vagina, making small incisions in your vagina before using stitches to repair or strengthen the tissue that supports the vagina. You will either have a spinal anaesthetic or a general anaesthetic for this procedure.
Hysterectomy – is usually only recommended for women with stage three or four uterine prolapse.
A hysterectomy can either be done entirely through your vagina with no cuts to your stomach, with a few small cuts to your stomach (laparoscopic or ‘keyhole’ hysterectomy) or with one long cut across your stomach (abdominal hysterectomy).
You will require a general anaesthetic and you will no longer be able to become pregnant after a hysterectomy.
Sacrocolpopexy – is a procedure where a piece of mesh is attached to your tailbone (sacrum) to give your vagina and/or uterus permanent support. It can either be performed as keyhole surgery or with one longer cut to your stomach (laparotomy) under a general anaesthetic.
Sacrocolpopexy is usually recommended for women with a stage three or stage four prolapse or for women who have already had a hysterectomy. It is also used as a uterus preserving prolapse surgery for younger women with a prolapsed uterus who don’t want to have a hysterectomy.
Colpocleisis – stitches a section of your vagina closed to prevent pelvic organs from moving into it. This operation has a very high success rate and it is performed vaginally without any incisions to your stomach.
Colpocleisis is a procedure usually reserved for older women because after this operation you can no longer have penetrative sex.
Manchester Operation – is a fertility preserving procedure which is associated with less blood loss and a faster recovery, when compared to vaginal hysterectomy.
Pelvic Organ Prolapse Surgery FAQs
A vaginal pessary is a soft removable plastic or silicone device that is inserted into your vagina to help support areas that are affected by pelvic organ prolapse, such as your vaginal walls and uterus.
Dr Siva will measure and fit the right size and type of pessary for you in his rooms. Ring pessaries can be removed and reinserted by you daily for cleaning or before sexual intercourse, while other types of pessaries will need to be removed and cleaned by Dr Siva in his rooms every 3 to 6 months.
It all depends on the type of prolapse surgery you are having. Most vaginal prolapse surgeries require just one or two nights stay in the hospital.
To reduce the risk of blood clots occurring in your legs you are encouraged to mobilise as soon as possible, usually the day after surgery. Spend some time each day going for a walk, slowly increasing as you feel comfortable. It is safe to go up and down stairs after prolapse surgery.
You will probably need extra help at home for the first 2 weeks as it’s important not to lift or bend too much at this stage.
Between 4 – 6 weeks post op you can start to move more, do gentle exercises and walk outside your home, slowly increasing your movement as you feel comfortable. At this stage you can:
- Hang small items of clothing on the line, but do not hang out heavy items or carry the washing basket.
- Go shopping and put small items into your shopping trolley, but have someone else push the trolley.
- Prepare and cook food on your stove, but avoid standing for long periods.
You may have a vaginal pack in your vagina after your vaginal prolapse surgery. A vaginal pack is a gauze pack placed in your vagina to prevent bleeding. Your vaginal pack will be removed within 24 hours of your surgery, before you are discharged from the hospital.
It is normal to experience some mild vaginal bleeding in the first week after surgery. If your bleeding is heavier than a period, itchy or if it is offensive smelling, please get in touch with Dr Siva as this may indicate a blood clot or an infection that you might need treatment for.
To prevent constipation, make sure you eat a well balanced diet with plenty of fibre and try to drink 2-3 litres of fluids a day. We also recommend regular stool softeners after surgery for about 2 weeks. If you experience ongoing constipation a laxative may help or you might need to get in touch with your GP or Dr Siva’s rooms.
It all depends on the type of vaginal prolapse surgery you have. Abdominal open surgery has a longer recovery time and it can take 4 – 6 weeks to fully heal. Keyhole (laparoscopic surgery) surgery has a shorter recovery time of approximately 1 – 2 weeks to recover. Vaginal surgery could take any time from 6 – 12 weeks duration.
- Tea, coffee and alcohol – they can make you urinate more often
- Strenuous tasks
- Standing still for long periods
- Lifting anything heavier than half a kettle of water
- Smoking – a ‘smoker’s cough’ can strain your pelvic floor muscles
- Weight gain – it can put pressure on your pelvic region
Do not place tampons or anything else in your vagina until after your post op visit with Dr Siva, which is usually 6 weeks after surgery..
You can resume driving once you can easily turn in your seat without discomfort and can safely perform an emergency stop – usually about 4 weeks after surgery. We highly recommend you see your GP prior to getting the clearance for driving.
The amount of time you need to take off work will depend on the type of vaginal prolapse surgery you have had.
You will probably need to take 6 – 12 weeks off work after vaginal prolapse surgery. This duration does depend on multiple factors. Please discuss this with Dr Siva prior to your hospital discharge.
Sexual intercourse can be resumed once you’ve healed completely and have no bleeding or discharge), which is usually after 12 weeks, however you may require additional lubrication and experience some discomfort .
ANY FURTHER QUESTIONS?
Please feel free to get in touch with Dr Siva’s rooms via email ipswichgyn@gmail.com or call (07) 3816 9189
for any further questions about our appointments, fees or anything else.